Successful Treatment of Typhoid Fever with a Single Dose of Ceftriaxone for One or Two Days*
Department of Internal Medicine, Catholic Medical College, Seoul, Korea
Address
Reprint requests: Hee Young Chung, M.D., Department of Internal
Medicine, Catholic Medical College, St. Mary’s Hospital, #62,
Youido-Dong, Young-dungpo-Gu, Seoul 150, Korea
*This work was presented in part at the 14th International Congress of Chemotherapy, held in Kyoto, Japan, 23–28 June 1985
Copyright © 1987 The Korean Association of Internal Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (
http://creativecommons.org/licenses/by-nc/3.0/)
which permits unrestricted noncommercial use, distribution, and
reproduction in any medium, provided the original work is properly
cited.
Abstract
The
therapeutic efficacy of ceftriaxone was evaluated in variable dose and
duration schedules in twenty patients with bacteriologically proven
typhoid fever. The results were satisfactory in the cases that were
given a single dose of 3 g for two days (12/12) or 4 g for one day
(3/4). Some untoward reactions were observed in 8 cases, but it was not
clinically significant.
Ceftriaxone
appears to be safe and effective in the treatment of typhoid fever when
administered in a single dose of 4 g for one day or 3 g for two days on
an outpatients basis.
Keywords: Ceftriaxone, Typhoid fever
INTRODUCTION
Chloramphenicol
has been the antibiotic of choice for patients with typhoid fever for
more than 30 years, although ampicillin and cotrimoxazole have been
introduced as alternatives, they have side effects, and disadvantages of
frequent administration and long duration of treatment similar to
chloramphenicol therapy.
Reports on the
usefulness of cephalosporin antibiotics (cefazolin, cefamandole,
cefotaxime, etc.) in the treatment of salmonella bacteremia have been
inconclusive1–3).
The purpose of this study was to determine whether the treatment of
typhoid fever with a single dose of ceftriaxone, given for one or two
days, is effective.
MATERIALS AND METHODS
During
a one-year period from February, 1984, to February, 1985, twenty
patients, 9 males and 11 females, ranging from 20 to 61 years of age
were studied. In every case, the clinical features were compatible with
typhoid fever and the diagnosis was confirmed by isolating salmonella
typhi from blood. None of the patients had any specific underlying
diseases or abnormal renal function. Ceftriaxone (F. Hoffmann-La Roche
Inc.) was administered by bolus injection to all patients as shown in .
Blood cultrues were repeated every other day until the patients were
discharged from the hospital. Tests for monitoring possible drug
toxicity included the white blood cell count and differential,
creatinine, bilirubin, liver function enzymes, and urinalysis.
Laboratory tests were performed before the beginning of therapy and
after discontinuation of therapy.
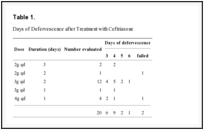
Days of Defervescence after Treatment with Ceftriaxone
RESULTS
shows the different dose and duration schedules of ceftriaxone which
was administered on a graduated varying basis, and the days of
defervescence.
The results were satisfactory except in
two cases, the ones who had a single dose of 4 g for one day
administered. Bacteremia cleared within one day after treatment in all
patients. In seventeen cases, stool cultures became negative within 7
days, however, in three, within 14 days.
Untoward
reactions were mild. The elevation of SGOT developed in three cases,
however, the authors were not able to determine whether this was
directly related to ceftriaxone or not. Nausea during injection was
noticed in two cases.
Pruritus, diarrhea, or flushing of face were observed in each one case respectively.
DISCUSSION
Ceftriaxone,
a new parenteral cepalosporin, has some properties which may make it
particularly useful in the treatment of typhoid fever.
First, it has excellent in-vitro activity against most clinical isolates of Salmonella spp.4), and also superiority over ampicillin and other cephalosporin in experimental Salmonella typhimurium infection.
Second,
it has a high level of biliary excretion. Increased biliary excretion
is desirable in the treatment of typhoid fever, because the gallbladder
contains a large number of bacilli and excretes them even in the acute
stage. The gallbladder also becomes a source of the organisms in chronic
carriers. In addition, it possesses a long serum half life which
permits single dose therapy in an inpatient or outpatient setting.
Initially,
the authors evaluated a single dose of 2 g for three, days in two
cases: the results were excellent. However, a single dose of 2 g for two
days failed in one case. So, the single dose of 3 g for two days was
evaluated in twelve cases. The fever subsided within four days in nine
cases and within six days in three cases ().
Although the single dose of 3 g for one day was successful in one case,
the dose was increased to 4 g in four cases, with satisfactory
responses being achieved in three cases (). It has been suggested that endogenous pyrogens released by local inflammatory effects of Salmonella typhi
endotoxin may sustain the pyrexia in typhoid fever. It dosen’t seem
likely that persistent high fever should be always related to the
organisms in the blood.
The effect of ceftriaxone in a patient who was given a single dose of 3g for two days.
The effect of ceftriaxone in a patient who was given a single dose of 4g for one day.
According
to our previous study, bacteremia cleared within one day after
intravenous injection of ampicillin or chloramphenicol in almost all
cases.
In this study, also bacteremia cleared within one day after treatment in all cases.
It is interesting the results were excellent inspite of the withdrawal of antibiotics during the persistent fever.
It is interesting that the results were excellent inspite of the withdrawal of antibiotics during the persistent fever.
Stool
cultures became negative within 14 days in all cases, but follow-up
cultures for the evaluation of chronic carriers could not be obtained.
There was no clinical evidence of relapse within eight weeks.
In
conclusion, this study gives support for the clinical efficacy of
ceftriaxone as a single dose of 3–4 g for one or two days, although
these regimen might be suitable for the treatment of patients with
typhoid fever on an outpatient basis, especially in developing countries
where there may be difficulties in admission.
It
would be reasonable to carry out clinical trials to assess the optimal
duration of treatment in other bacterial infectious diseases in normal
host.
REFERENCES
1.
Uwaydah E. Cefazolin in the treatment of acute enteric fever. Antimicrob Agents Chemother. 7976;10:52. [PMC free article] [PubMed]2.
Uwaydah M, Nassar NT, Harakeh H, Vartivarian S, Talhouk A, Kantrajian H. Treatment of typhoid fever with cefamandole. Antimicrob Agents Chemother. 1984;26:426. [PMC free article] [PubMed]3. Park
SC, Lee CH, Seok SE, Kim TW, Park CH, Chung SK, Kim SY, Choi HS, Choi
HR, Lee MA. Clinical trial of cefotaxime in patients with typhoid
fevcer. Korean J Infect Dis. 1981;16:8.
4.
Chau
PY, Ng WS, Ling J, Arnold K. In vitro susceptibility of Salmonella to
various antimicrobial agents, including a new cephalosporin, Ro 13-9904.
Anbtimicrob Agents Chemother. 1981;19:8. [PMC free article] [PubMed]5.
Patel IH, Kaplan SA. Pharmacokinetic profile of ceftriaxone in man. Am J Med. 1984;77:17. [PubMed]6.
Hornick
RB, Greisman Se, Woodward TE, Dupont HL, Dawkins AT, Snyder MJ. Typhoid
fever: pathogenesis and immunologic control (first of two parts) N Engl J Med. 1970;283:686. [PubMed]7.
Zhou HH, Chan YPB, Arnold K, Sun M. Single-dose pharmacokinetics of ceftriaxone in healthy Chinese adults. Antimicro Agents Chemother. 1985;27:192. [PMC free article] [PubMed]8.
Hoffman
TA, Ruiz CJ, Counts GW, Sachs JM, Nitzkin JL. Waterborne typhoid fever
in Dade County, Florida. Clinical and therapeutic evaluation of 105
bacteremia patients. Am J Med. 1975;59:481. [PubMed]9. Kim
YM, Chung HY. Disappearance of Salmonella typhi in peripheral blood of
typhoid fever after administration of ampicllin or chloramphenicol. Journal of Catholic Medical College (Seoul) 1981;34:474.

 Facebook
Facebook
 Twitter
Twitter
 Google+
Google+